Kenya’s pursuit of Universal Health Coverage (UHC) has lacked a comprehensive assessment of its mixed health system, limiting the ability to address critical gaps and seize growth opportunities. This has led to key challenges in healthcare delivery remaining unclear, and the misalignment of the allocation of resources in comparison with actual needs. The public sector, serving as the primary healthcare provider for low-income populations, has frequently been overburdened, with limited visibility on where collaboration with the private sector could ease these pressures. Meanwhile, the private sector, which plays a crucial role in expanding access, lacked a unified framework to effectively integrate its services with national health goals. This disconnect has resulted in service gaps and inefficiencies that adversely impact patient outcomes.
The newly released 2024 State of Kenya’s Health Market report bridges this gap, providing a crucial analysis of Kenya’s health system and identifying actionable reforms to enhance healthcare delivery and accessibility across public and private sectors. Conducted by the Ministry of Health in collaboration with the USAID Private Sector Engagement (PSE) Program, this comprehensive assessment focuses on six priority counties—Nairobi, Kisumu, Uasin Gishu, Homa Bay, Nakuru, and Mombasa—highlighting both pressing challenges and opportunities for meaningful improvement.
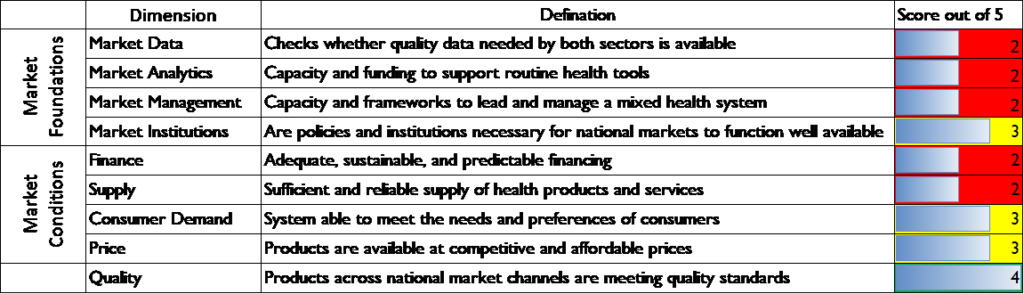
Figure 20: Health Market Assessment Results
One of the central findings is the need for stronger coordination among national and county-level healthcare providers. Sylvia Wamuhu, Chief of Party for the USAID PSE Program, emphasized during the report launch that “a shift toward greater health market coordination will result in improved oversight, better decision-making, and sustained growth in Kenya’s health sector.” Dr. Martin Sirengo from the Directorate of Health Sector Coordination echoed these sentiments, adding, “Enhancing management and stewardship across the health value chain and strengthening collaboration between national and county governance structures highlight the importance of a coordinated approach that engages all stakeholders to ensure an integrated and effective health system.” These insights emphasize the need for unified governance in building an efficient and effective healthcare system for Kenyans.
A significant issue identified in the report is the fragmented coordination between national and county health systems. Although Kenya’s healthcare market comprises a mix of public and private, coordination at the county level is inconsistent, leading to uneven service delivery. Strengthening governance and aligning efforts between county and national governments is essential to improving healthcare outcomes.
The report also points to limited data sharing between public and private sectors, which hinders healthcare planning and decision-making. Inaccessible market data within the private sector has created an information gap, impeding effective healthcare solutions. Without a comprehensive picture of healthcare demand and supply, resource allocation remains challenging. The report advocates for establishing robust data-sharing frameworks to improve transparency and collaboration, thus facilitating more informed decision-making and resource distribution across healthcare systems.
Financial constraints and supply chain challenges remain significant strains on Kenya’s healthcare system. Despite government efforts to allocate about 11% of the national budget to health, the system remains heavily reliant on donor funding for its development budget. Supply chain inefficiencies further disrupt service delivery, with frequent stockouts impacting access to affordable healthcare. The report notes that the successful implementation of Social Health Insurance (SHI) could enhance insurance coverage, reduce reliance on donor funding, and improve access to care, especially in marginalized regions.
The report highlights the underutilized potential of Kenya’s local manufacturing sector. Although mandatory SHI could stimulate demand for locally produced health products and services, the current production capacity remains limited. The absence of price control policies also impedes the provision of affordable, locally manufactured medicines. At the launch, Jane Ngugi, the USAID PSE Program’s Agreement Officer’s Representative, stated, “The additional measures that development partners like USAID and others are exploring to bolster Kenya’s journey toward self-reliance—including efforts to enhance commodity security and expand local manufacturing—are deeply appreciated.” Expanding local pharmaceutical manufacturing would reduce dependence on imports, lower healthcare costs, and create jobs, fostering economic resilience in the health sector.
Private healthcare providers are often perceived as offering higher-quality services, yet smaller private entities struggle with operational challenges due to high costs and low revenues, creating inequities in service delivery. To address this, the report calls for implementing a unified healthcare quality policy, such as the Kenya Quality Model for Health (KQMH), to ensure consistent standards of care across all healthcare providers. This would promote equitable access to quality healthcare nationwide.
The report emphasizes the need for comprehensive data on healthcare demand and sociodemographic factors. National data on demand remains limited to specific health programs, and with only 26% of Kenyans having insurance—many in the informal sector with dormant coverage—access to care remains constrained for much of the population. The report recommends policies that address these gaps in service delivery, product availability, and technology utilization.