Concurrent partners
PS Kenya in collaboration with the Government of Kenya developed communication dissuading couples from engaging in concurrent sexual partnerships popularly known as Mpango wa Kando communication. The communication sought to create understanding on:
- How a large number of otherwise unrelated individuals can be connected sexually in a network of concurrent relationships
- How the infection of one individual in the network with HIV can result in the rapid transmission of the virus to individuals throughout the network
An appreciation of concurrency as one of the primary behaviors contributing to the high incidence of HIV among relationships previously considered “low risk”
Alcohol influence “Kunywa Zaidi, Teleza Zaidi”
The message served as a rallying call, urging individuals to reject social norms that would increase the risk of contracting HIV. It emphasized that higher alcohol consumption correlated with an elevated likelihood of engaging in risky sexual behaviour, thereby heightening the risk of HIV transmission. This message was tailored for both single and married males and females aged between 18 and 30 years.
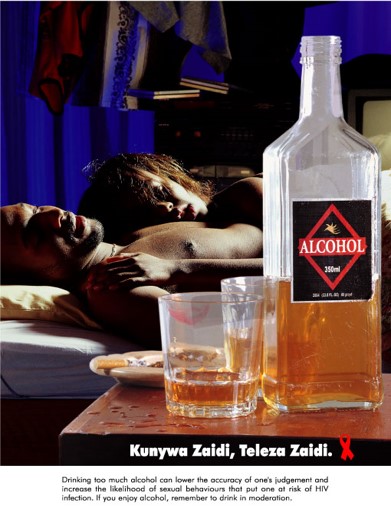
The target audience included three main groups: sporadic heavy drinkers, frequent heavy drinkers, and social drinkers along with friends of drinkers. By reaching out to these individuals, the campaign aimed to raise awareness about the link between alcohol consumption and risky sexual behaviour, ultimately reducing the incidence of HIV transmission within the community.




